Better outcomes and cost savings with intentional care transitions plan
With a long-standing commitment to providing safe, high-quality and effective care across the continuum, a large health system in the Midwest understood that a significant number of patients will always require post-discharge support.
Even with excellent care and intensive discharge preparation, factors such as the patient’s current health condition and circumstances such as unemployment, lack of insurance, or the inability to access a primary–care provider often trigger the need for additional support.
A decentralized post-discharge call process, reliant on already busy units, required significant staff time away from the bedside and was resulting in a non-standard process for resolving patient issues or sharing information that was gathered during calls.
Opportunity
Leaders recognized a need to develop programs and services that would enable them to provide more personalized post–discharge care, increase access, and reduce readmissions. As part of its overall readmission strategy, the health system appointed a multi-disciplinary team, which identified several areas of focus:
Address the needs of high-risk patients with chronic health conditions
To reduce the frequency of readmissions as the result of the severity of illness or the inability to manage their conditions outside the hospital, the team revamped the Heart Failure Program to offer home–based health and palliative care and created Community Cares to provide home-based APRN provider visits to patients with chronic obstructive pulmonary disorder (COPD).
Target a broader population of patients
The team established the Transitional Care Clinic to provide post-discharge healthcare to patients without access to primary-care providers. Although the majority of the patients treated in the clinic do not impact readmission penalties, Leaders felt that it was imperative to make these patients part of their care strategy to better address the needs of underserved patients in their community—with the right care in the right setting.
Implement a mechanism to catch patients who fall through the cracks
To ensure that patients get the post-discharge support they need—consistently and efficiently—and that they are placed in the appropriate program for ongoing care, a centralized process and discharge–call program needed to be implemented as well.
100%
OF PATIENTS CONTACTED
AFTER CONNECT
93%
REDUCTION
IN READMISSIONS
$1.6 million
COST
SAVINGS
Solution
To successfully achieve its goals, the health system combined the resources of its Transitional Care Clinic with a standardized, centralized discharge-call process utilizing NRC Health’s Transitions.
The facility-based Transitional Care Clinic is staffed with a team that includes a nurse, a medical assistant, an APRN, and a social worker, who provide care to patients without a primary–care provider. The clinic is a key component of the patient discharge planning process. If a patient does not have a provider or cannot be seen by their provider or a specialist, the patient is scheduled for an appointment at the clinic. This reduces the likelihood of the patient seeking care in the emergency department or allowing their condition to worsen, thus increasing the risk of hospital readmission.
The team of healthcare providers then follows the patient through their care plan for up to 45 days. The team works to stabilize the patient’s health condition and assists in identifying the psychosocial determinants of health, such as access to insurance (completing Medicaid applications); community resources for basic needs like utilities, transportation, and housing; obtaining and managing medications; managing acute and chronic health problems; and health education.
A major goal is to teach the patient to manage and be responsible for their own health conditions. An important aspect of this is working with patients and providers within the community to ensure that each patient has a primary-care physician for future healthcare needs.
While the availability of healthcare services and support through the Transitional Care Clinic is critical, so is the ability to identify the patients that require these services post–discharge and those who are experiencing obstacles in accessing care. That’s where NRC Health was able to make a difference, as part of the system-wide, centralized discharge–call program leaders that implemented to contact all patients, resolve clinical and service issues, and collect information to improve the delivery of care.
As patients are discharged, they are told they will receive a follow–up call as part of their care plan and the importance of participating in that call. Within 72 hours of discharge, the patient receives a quick phone call and is asked five questions to determine if they need additional help from care teams due to health status or inability to comply with their care plan. Should a patient self-select that they do need additional support, the system is immediately notified to contact that patient.
The process ensures that 100% of patients are contacted consistently and that at-risk patients are identified and triaged back to care teams for follow–up. On average, less than 17% of patients require follow-up.
Goals of Transitional Care Clinic for the patient
Stabilize the patient’s condition
Educate the patient on how to manage their condition
Provide resources to empower the patient to take control of their condition and healthcare needs, including:
- Financial counseling
- Medication assistance
- Access to medical equipment
Aquire a primary care physician for the patient
Integrating discharge calls into the Transitional Care Clinic
The integration of the Transitions clinical and service–recovery process into the Transitional Care Clinic is vital to the success of the health system’s program. To address the follow-up with the small percentage of patients discharged, a part-time RN Care Coordinator position was created.
Transitions makes the initial outreach calls to patients daily between 11 a.m. and 1 p.m. The RN has immediate access to the list of patients requiring follow-up, and can see why follow-up is needed, then prioritize calls for the patients most in need of additional support.
As the nurse communicates with patients, they are able to quickly answer questions, assist with prescriptions, coordinate follow-up care, and provide service recovery if needed.
What’s more, all information gathered from the initial Transitions calls and the RN’s follow–up is tracked in the organizations NRC Health platform. Leadership and staff then have access to reporting tools that identify where things are working well in the hospital, as well as where gaps exist in the delivery of care.
The process utilizes Transitions both to find patients who fall through the cracks and identify process errors at the provider, unit, and hospital levels. As a result, the health system not only resolves current patient needs, but also uses patient issues and concerns to improve the delivery of care for future patients.
“The Transitional Clinic empowers patients to take control and manage their health care and condition. As a result, our patients get healthier, readmissions rates have declined, and we have been able to reduce unnecessary utilization of the most expensive settings of healthcare.”
—Senior Director, Operations
Outcomes
Within the first nine months of the program, Transitions contacted nearly 19,000 patients and identified 3,200 patients needing additional follow-up from care teams. Without these calls and access to the RN Care Coordinator, it is likely that many of these patients would have experienced health issues, resulting in a longer recovery period or complications leading to an emergency-department visit or readmission. Leaders can attribute the reduction in overall readmissions in part to Transitions, because data supports that patients participating in the Transitions call have an average readmission rate of 5%, while those who don’t have a 9% readmission rate.
Having a centralized process in place is also helping the health system drive process improvement, so the care provided at the bedside continues to excel. By spending time with patients who have issues post–discharge, the RN Care Coordinator is able to provide more personalized post–discharge care and identify trends, pitfalls, and gaps in the delivery of care. The RN is able to analyze this information and make process–improvement recommendations based on patient feedback regarding care delivery and the discharge process.
The results are remarkable: readmission rates are lower, HCAHPS scores are higher, and most importantly, patients have greater trust and confidence in their relationship with the health system.
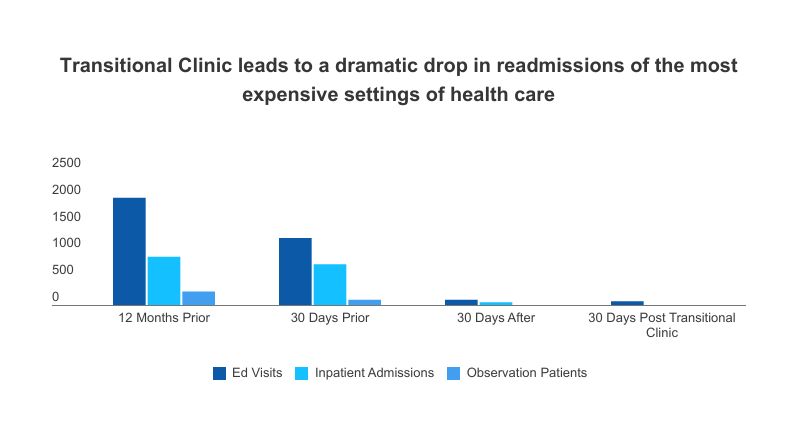
The Transitional Care Clinic is also an important part of that story. Funded in full by the health system at a cost of $300,000 a year for clinic staffing, the investment has already seen a significant return in both readmissions and financial outcomes.
Comparing patient healthcare usage in the clinic this year to the previous year, leaders saw a 93% reduction in the utilization of the emergency department and inpatient care by these patients.
At an average cost of $1,932 per patient to utilize these healthcare settings, the reduction in readmissions resulted in an estimated $1.6 million cost avoidance for the health system.
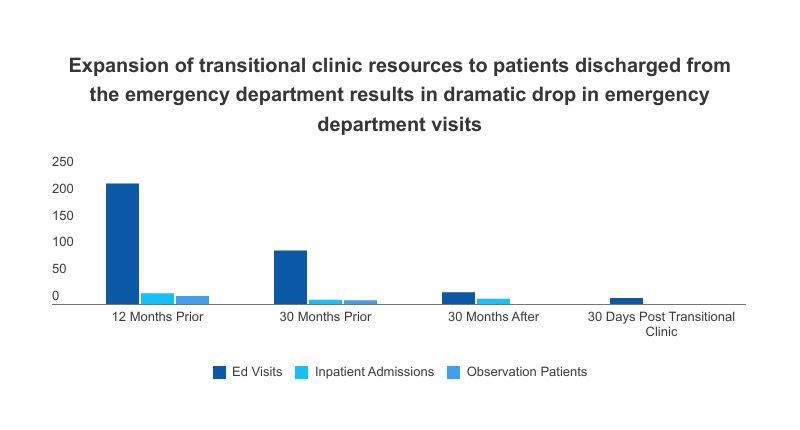
To further reduce unnecessary emergency-department visits, the health system expanded Transitional Care Clinic resources to include patients discharged from the emergency room.
These patients receive a follow-up medical call with access to an appointment at the clinic. The goals remain consistent with the inpatient population—to stabilize the patient’s condition, to empower them to manage their condition, and to connect them with a primary-care physician to serve their non-emergency healthcare needs. In a matter of months, simply reaching out to these patients at discharge has resulted in a 98% reduction of emergency visits.
While these savings alone would be reason enough for the average healthcare system to continue operating the clinic, the health system proves it is definitely above average. When asked, staff and leadership said they are prouder of the hundreds of patients who now receive better–quality care and live healthier lives.
“If the shared goal of all healthcare organizations is to provide the right care for patients, then tools like these are as vital to an organization as oxygen is to patients.”
—RN Care Coordinator
Learn more about NRC Health’s platform here or call 800.388.4264.
Let's Get Social
Want to follow the Human Understanding movement? Check out NRC Health on social media.